Biocompatible Materials in Restorative Dentistry: Innovations and Applications
The field of dentistry has witnessed exponential growth in the last few decades, paving the way for significant advancements and innovations in dental materials. The pivot towards biocompatible materials underscores the commitment of the dental industry to improve patient safety and treatment outcomes.
Biocompatible materials in dentistry are substances designed to interact with the human body without eliciting adverse reactions. Their application in restorative dentistry ranges from dental filling material to dental implant material, all of which have one thing in common: compatibility with the patient’s biology.

The importance of biocompatibility in restorative dentistry cannot be overstated. From basic dental materials to more complex ones used in procedures such as dental bone grafts, ensuring the materials are biocompatible significantly impacts the success of the treatment and the patient’s overall health.
In this blog, we dive into the world of biocompatible materials in dentistry, examining the latest innovations and their practical applications.
Understanding Biocompatibility
Before we delve into the specific materials, it’s crucial to understand what makes a dental material biocompatible. This is closely tied to the physical properties of dental materials and their mechanical properties. Essentially, a biocompatible material should not cause any harmful reactions or irritation in the patient’s body. They should also mimic the natural structures they replace in terms of function and aesthetics.
For example, a dental filling material needs to withstand the forces of chewing, blend in with the natural color of the teeth, and not cause any allergic reactions. Similarly, dental implant materials should encourage bone growth around them, creating a secure base for the implant, and should not trigger any immune response.
Innovations in Biocompatible Materials
The drive for safer, more effective treatments has seen the development of innovative materials that satisfy these stringent criteria. Here are some recent innovations:
Dental Composite Materials: These are tooth-colored materials composed of resin and glass or ceramic particles. They’ve become the gold standard for dental filling material due to their excellent biocompatibility, aesthetic appeal, and durability. The composition of these materials has been refined over the years to improve their physical and mechanical properties.

Dental Implant Materials: Titanium and titanium alloys have been the preferred choice due to their superior biocompatibility, mechanical strength, and corrosion resistance. Recently, ceramic materials like zirconia are gaining popularity as they offer excellent biocompatibility, aesthetics, and power, making them a promising dental implant material.

Dental Bone Graft Materials: Bone graft materials derived from human or animal sources are highly biocompatible and promote bone growth. Synthetic options, made from biocompatible materials like hydroxyapatite and tricalcium phosphate, are also widely used.
Dental Impression Materials: Silicone-based materials, known for their exceptional detail reproduction, dimensional stability, and biocompatibility, dominate this category.

Suppliers and Journal Resources
Finding reliable dental material suppliers and staying updated with the latest research can be challenging. For suppliers, look for companies with a solid reputation in the industry and positive feedback from dentists. As for research, the Dental Materials Journal is a reputable source of cutting-edge findings. Its impact factor – a measure of the frequency with which the average article in a journal has been cited in a particular year – is a testament to its influence on dental materials research.
Understanding Biocompatible Materials in Dentistry
In the ever-evolving world of dentistry, one term you’ll frequently come across is ‘biocompatible materials.’ These materials used in various therapeutic procedures represent a significant leap forward in dental treatment. But what exactly are they, and why are they so essential? Let’s delve in to find out more.
Defining Biocompatible Materials: Biocompatible materials, by definition, are those that can exist or perform their intended function without causing any harm to living tissues. In essence, they are ‘friendly’ to the body. In dentistry, these are materials used in restorative procedures that will not cause adverse reactions when they come into contact with a patient’s oral tissues.
Several vital characteristics set biocompatible materials apart:
Non-Toxic: Biocompatible materials must not release any harmful substances into the body. This is a critical factor, given that dental materials often remain in the body for extended periods.

Non-Carcinogenic: Biocompatible materials must not induce cell mutations or lead to cancerous growths.
Non-Allergenic: Allergies can be an issue with certain dental materials. Biocompatible materials are selected to minimize allergic reactions.
Bio-inert or Bioactive: Depending on their application, biocompatible materials can either be bio-inert, meaning they do not interact with surrounding tissues, or bioactive, meaning they can interact positively with body tissues, promoting healing or integration.

The Importance of Biocompatibility in Dental Restorations
Biocompatibility is paramount in dental restorations for a simple reason: to prevent adverse reactions that could impact the patient’s overall health. Responses could range from allergies and sensitivities to more severe systemic reactions. Thus, the importance of biocompatibility cannot be overstated. It ensures that restorations will not only serve their mechanical function but also contribute to the patient’s overall well-being.
Common Biocompatible Materials in Restorative Dentistry
Several types of biocompatible materials have found widespread application in restorative dentistry. These include:
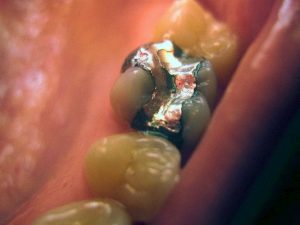
Amalgam: A mixture of mercury and metal alloy, dental amalgam has been used for over a century due to its durability and ease of use. However, its use has decreased due to aesthetic considerations and concerns about mercury exposure.
Composite Resins: These tooth-colored materials have excellent aesthetic properties and are highly biocompatible. They can mimic the natural appearance of teeth and are commonly used for fillings, veneers, and bonding.

Ceramics: Dental ceramics, like porcelain and zirconia, are incredibly versatile. They offer excellent aesthetics, strength, and biocompatibility, making them ideal for crowns, bridges, and implants.

Titanium and Titanium Alloys: Titanium is the material of choice for dental implants due to its excellent biocompatibility, strength, and ability to Osseo integrate, or fuse, with bone.

Biocompatibility of Dental Materials
As a field, dentistry has come a long way from the traditional materials that were once the standard. Biocompatible materials are setting a new standard in patient safety and comfort. Biocompatibility remains at the core as we navigate the world of dental materials.
Understanding Biocompatibility in Dental Materials
In dentistry, biocompatibility pertains to the ability of a material to perform with an appropriate host response when applied. Biocompatible dental materials should not cause adverse reactions when used in the oral cavity, ensuring the patient’s overall safety and comfort.
Biocompatibility is multi-dimensional, encompassing various biological interactions, such as immunological, toxicological, and tissue responses to dental materials. As such, the biocompatibility of dental materials is not a ‘one size fits all’; it varies, depending on numerous factors.
Factors Influencing the Biocompatibility of Dental Materials
The biocompatibility of dental materials can be influenced by several factors, including:
Composition of the Material: Different materials have different documents, leading to variations in their reactions with oral tissues.
Placement Site: The location of the material can impact its biocompatibility. For instance, biocompatible material in the mouth’s hard tissues may not be suitable for soft tissues.
Duration of Exposure: The longer a material stays in the body, the higher the chance of triggering a biological response.
Patient’s Health Status: A patient’s overall health, immune response and specific allergies can significantly affect a material’s biocompatibility. Material Processing and Handling: How a material is processed, sterilized, and handled can impact biocompatibility.

The Importance of Choosing Biocompatible Dental Materials
Selecting biocompatible materials for dental restorations is more than just a best practice—it’s a duty to the patient’s health and safety. Biocompatible materials can help reduce potential allergic reactions, minimize toxicity, and improve the overall patient experience.
Moreover, biocompatible materials often lead to better clinical outcomes. They can enhance healing, reduce inflammation, and promote integration with the surrounding tissues.
In essence, the right choice of biocompatible dental materials plays a pivotal role in the long-term success of dental restorations. As dental professionals, understanding the nuances of these materials and making informed choices can significantly impact our ability to deliver safe, effective, and patient-friendly dental care.
Dental Filling Materials and Biocompatibility
As we delve deeper into restorative dentistry, dental filling materials unquestionably hold significant importance. Chosen for their durability, appearance, and biocompatibility, these materials have come to define the success of dental restorations.
Understanding Dental Filling Materials
Dental filling materials, as the name suggests, are used to fill cavities or repair worn, decayed, or damaged teeth. The choice of dental filling material can significantly impact the treatment outcome, influencing longevity, aesthetics, and patient comfort.
Besides their mechanical properties and aesthetics, the critical characteristic of dental filling materials is their biocompatibility. Given that these materials interact directly with the oral tissues, they must be biocompatible, causing minimal adverse reactions, if any.

Biocompatibility Considerations for Dental Filling Materials
Choosing biocompatible dental filling materials is a multifaceted decision. Here are some of the considerations:
Physical and Mechanical Properties: The filling material must be robust enough to withstand the forces of biting and chewing. Additionally, it should resist wear and tear over time.
Chemical Stability: A biocompatible filling material should not leach harmful substances into the oral environment, posing a risk to the patient’s health.
Aesthetics: While not directly related to biocompatibility, aesthetics significantly influence patient satisfaction and treatment acceptance.
Adherence: The material must bond effectively with the tooth structure, which can help prevent leakage and recurrent decay.
Biocompatible Dental Filling Materials and Their Applications
Several biocompatible materials are used as dental fillings, each with its own set of advantages:
Composite Resins: These are tooth-colored materials preferred for their aesthetics and ability to bond directly to the tooth structure. Their composition, mainly a blend of a resin matrix and glass filler particles, offers good strength and durability.
Glass Ionomer blocks of cement: Known for their fluoride-releasing properties, these materials are often used in children and root caries in older adults. They have a strong bond with tooth structure and offer chemical stability.
Porcelain (Ceramic) Fillings: These are durable and aesthetically pleasing, making them suitable for visible teeth. They are resistant to staining and are highly biocompatible.
Gold Fillings: Although not expected due to their high cost and visible color, they are durable and have high biocompatibility.
Dental Impression Materials and Biocompatibility
Impressions in dentistry have always been vital, serving as the foundational blueprint for numerous restorative works, prosthetics, and diagnostic models. Given their critical role, the biocompatibility of these impression materials holds paramount significance.
The Role of Dental Impression Materials in Restorative Dentistry
Dental impression materials capture a detailed 3D replica of a patient’s teeth and oral tissues as a template for fabricating crowns, bridges, dentures, and other dental restorations. They can also be used to create diagnostic and treatment planning models.
The accuracy of an impression directly affects the fit and function of the resulting restoration, making the choice of impression material crucial. However, their biocompatibility is paramount as these materials come into direct contact with the oral tissues.
Biocompatibility Factors in Dental Impression Materials
Selecting a biocompatible dental impression material involves consideration of the following aspects:
Tissue Reaction: The material should not cause adverse reactions such as inflammation or allergy when it comes into contact with the oral tissues. The absence of toxic substances in the composition of the material is crucial.
Mutagenicity and Carcinogenicity: Dental impression materials should not have mutagenic or carcinogenic properties, i.e., they should not cause genetic mutations or promote cancer development.
Absence of Harmful By-products: Some fabrics may produce harmful by-products during setting or storage. These by-products should be minimal and not pose any health risks.
Biocompatible Dental Impression Materials
Several dental impression materials balance the need for accuracy and biocompatibility:
Alginate: This seaweed-based material is extensively used for preliminary impressions. It is non-toxic, non-irritant, and inexpensive, making it a popular choice in dental clinics.
Silicone-Based Materials: These are condensation silicones and addition silicones (polyvinyl siloxanes). They offer excellent dimensional stability and detail reproduction and are non-irritant to tissues.
Polyether Impression Materials: Known for their excellent detail reproduction, oral tissues also well-tolerated these materials. However, they might be slightly more rigid than silicone materials, making removal from the mouth more challenging.
Zinc Oxide Eugenol (ZOE): While primarily used in endodontics, ZOE can also be used as an impression material. Its soothing properties make it highly biocompatible, but it’s worth noting that some patients may be allergic to eugenol.
In conclusion, dentists must balance the mechanical properties required for accurate impressions and the biocompatibility necessary for patient safety. Understanding the different dental impression materials and their biocompatibility can guide dentists in making an informed choice, leading to better outcomes in restorative dentistry.
Dental Composite Materials and Biocompatibility
Dental composite materials are tooth-coloured restorative materials primarily used in direct dental restorations, including fillings and veneers. Their versatile nature and ability to closely match the appearance of natural teeth have made them a popular choice among dentists and patients alike.
The composition of these materials is complex, with a blend of resin matrix and inorganic filler particles. The resins usually contain monomers like Bisphenol A-glycidyl methacrylate (Bis-GMA) or Urethane dimethacrylate (UDMA), while the fillers may consist of silica, quartz, or glass particles.
Biocompatibility and Dental Composite Materials
The biocompatibility of dental composite materials revolves around these primary considerations:
Monomer Release: Over time, unreacted monomers can be released into the oral environment. Though the amount is generally small, they could cause allergic reactions in sensitive individuals.
Cytotoxicity: Dental composites should exhibit minimal cytotoxicity, i.e., not harming the living cells in the pulp or surrounding tissues.
Erogenicity: Some concerns about the potential estrogenic effects of Bis-GMA-based resins have been raised. However, current research suggests that the levels released in the oral cavity are significantly below those required to exert such effects.
Biocompatible Dental Composite Materials
Several dental composite materials marry the need for aesthetics, strength, and biocompatibility:
Nano-Hybrid Composites: These composites blend different-sized filler particles, offering excellent aesthetics, durability, and lower polymerization shrinkage. They’re generally well-tolerated by the oral tissues.
Bulk-Fill Composites: Designed to simplify the filling process, these materials can be placed in larger increments while maintaining a good depth of cure. They exhibit good biocompatibility with minimal cytotoxicity.
Bioactive Composites: These innovative materials not only serve as passive restorations but also actively release ions like calcium, phosphate, and fluoride, which can remineralize tooth structure and inhibit caries. They represent a promising direction in the development of biocompatible dental materials.
Dental Implant Materials and Biocompatibility
Biocompatibility plays a fundamental role when choosing materials for dental implants. Given that these materials are intended to interact with living bone tissue, they must be mechanically reliable and foster an optimal biological response. In this section, we delve into the significance of biocompatibility in dental implant materials, explore commonly used materials, and discuss the long-term success rates of dental implants concerning their biocompatibility.

The Importance of Biocompatibility in Dental Implant Materials
Dental implants are a staple in restorative dentistry, providing a stable and durable solution for missing teeth. These devices interface directly with the jawbone, making the choice of material crucial for their success. Biocompatible materials are paramount because they must:
Promote Osseointegration: Dental implant materials should encourage the growth and integration of the surrounding bone tissue, a process known as osseointegration, without eliciting an adverse biological response.
Resist Corrosion: Given their long-term placement within the body, these materials must resist corrosion to prevent the release of harmful ions or particles into the surrounding tissue.
Sustain Mechanical Loads: Materials must be capable of withstanding the substantial mechanical loads produced during chewing.
Biocompatible Materials Commonly Used for Dental Implants
Various biocompatible materials have been employed in dental implants. However, titanium and its alloys have been the gold standard for several decades. Here are a few commonly used materials:
Titanium and Titanium Alloys: Known for their excellent mechanical properties and biocompatibility, titanium is the most widely used material for dental implants. It promotes osseointegration and exhibits good corrosion resistance.
Zirconia: Zirconia, a ceramic material, is gaining popularity as a metal-free alternative to titanium. It is appreciated for its excellent biocompatibility, aesthetic appearance (as it is white and mimics a tooth’s color), and mechanical strength.
PEEK (Polyetheretherketone): A high-performance polymer, PEEK is a newcomer in dental implants, boasting high biocompatibility and flexibility similar to natural bone.
Long-term Biocompatibility and Success Rates of Dental Implants
Research and clinical experience have shown dental implants to have high long-term success rates, largely thanks to the biocompatible materials used. Titanium implants, for instance, demonstrate success rates above 90% over ten years, with similar figures reported for zirconia implants.
These high success rates are primarily due to excellent osseointegration, with the chosen materials providing a stable and biocompatible scaffold for bone growth. Furthermore, dental implants’ biocompatibility contributes to the low incidence of complications such as peri-implantitis or adverse tissue reactions.
Physical and Mechanical Properties of Dental Materials
In dentistry, the success of treatments and restorations depends heavily on the materials we use. While biocompatibility is a critical feature, it is not the only property of significance. Dental materials’ physical and mechanical properties play a fundamental role in their overall performance and the success of dental procedures. Let’s delve into these properties, their connection to biocompatibility and clinical performance, and some examples of dental materials boasting desirable characteristics.
The Physical and Mechanical Characteristics of Dental Materials
The physical and mechanical properties of dental materials refer to how these materials behave under various conditions and forces. Here are a few crucial ones:
Strength: Materials must be strong enough to withstand the forces of biting and chewing without fracturing.
Toughness: Dental materials must resist cracking and withstand heavy cyclic loads.
Elasticity and Plasticity: Dental materials should have a degree of flexibility to avoid stress concentration and fracturing.
Thermal Conductivity: Dental materials must insulate against temperature changes to avoid tooth sensitivity.
Hardness and Wear Resistance: Materials should resist wearing to maintain their function and aesthetics over time.
The Relationship Between Physical/Mechanical Properties and Biocompatibility
Dental materials’ physical and mechanical properties are closely tied to their biocompatibility and clinical performance. Material may be perfectly biocompatible but fail due to poor mechanical properties. On the other hand, a material with excellent mechanical properties might lead to biological complications if not biocompatible.
For example, a dental filling material must have the strength to withstand masticatory forces, but it is unsuitable for use if it causes an adverse biological reaction. Therefore, it is essential to balance these properties when selecting a dental material.
Examples of Dental Materials with Desirable Physical and Mechanical Properties
There are many examples of dental materials that have been developed with an optimal combination of physical, mechanical, and biocompatible properties:
Amalgam: Although its usage has declined due to aesthetic considerations and concerns about mercury, dental amalgam has been a reliable dental filling material for years, known for its strength, durability, and wear resistance.
Composite Resin: Composite resins, made from a mix of plastic and glass or ceramic, offer good strength, aesthetic appearance, and excellent bonding to the tooth structure.
Dental Ceramics: Used for crowns, bridges, and veneers, dental ceramics provide superior aesthetics, excellent biocompatibility, and good mechanical properties, including hardness and wear resistance.
Titanium: A popular material for dental implants due to its superb strength, corrosion resistance, and biocompatibility.
Dental Materials Online: Availability and Considerations
In today’s fast-paced digital world, more and more dentists are turning to online platforms to purchase dental materials. This shift has transformed the dental industry, enabling practitioners to compare and choose from a wide range of products at the click of a button. However, with this convenience come unique considerations and challenges, especially concerning the biocompatibility of materials. In this segment, we’ll explore the availability of dental materials online, concerns about their purchase, and tips for selecting reliable suppliers.
The Availability of Dental Materials Online
Online marketplaces have become a go-to source for various dental materials, from basic supplies to specialized equipment. Dental filling materials, dental impression materials, dental composite materials, dental implants, and more are all readily available from various online suppliers. This online availability offers dentists unparalleled convenience and choice, helping them find the best materials to suit their practice’s needs.
Considerations When Purchasing Dental Materials Online
While the online marketplace offers vast choices, it also presents unique considerations. Here are a few:
Biocompatibility: Always look for materials that are biocompatible to ensure patient safety. Check for indicators of biocompatibility, such as ISO certifications or FDA approvals.
Quality and Authenticity: Be cautious of counterfeit or substandard products. Always check product reviews and seller ratings, and ensure the product has a proper warranty.
Product Information: Detailed product descriptions and specifications are essential. A lack of information can lead to a better understanding of the product’s capabilities and proper usage.
Return Policy: A clear return policy is critical. If a product doesn’t meet your expectations or arrives damaged, you need the option to return or exchange it.
Tips for Selecting Reliable Dental Material Suppliers
Choosing the right supplier can significantly affect the quality of the materials you purchase. Here are some tips:
Reputation and Reliability: Look for suppliers with positive customer reviews and a good track record. They are more likely to provide quality products and reliable customer service.
Range of Products: Choose suppliers who offer a wide range of products. This could save you time and money, as you can purchase multiple items from a single source.
Transparency: Suppliers should provide clear, detailed product information, including specifications, origin, certifications, and warranty details.
Customer Support: Look for suppliers who offer robust customer support, ready to answer your queries and resolve any issues you may encounter.
Dental Restoration Materials and Biocompatibility
Restorative dentistry is essential in oral healthcare, addressing many dental issues, from tooth decay to tooth loss. The heart of restorative dentistry lies in the materials used to mimic natural teeth’ appearance, structure, and function. This section overviews dental restoration materials, discusses their role, highlights biocompatibility considerations, and shares examples of biocompatible materials commonly used in restorative dentistry.
The Role of Dental Restoration Materials in Restorative Dentistry
Restorative dentistry is a field that focuses on restoring the function and aesthetics of the oral cavity. It covers various treatments, including fillings, crowns, bridges, implants, and dentures. The success of these treatments largely depends on the dental materials used. The suitable materials replicate the natural appearance of teeth and stand up to the rigors of daily wear and tear, including biting, chewing, and temperature changes.
Biocompatibility Considerations in Dental Restoration Materials
Biocompatibility is a crucial factor when choosing dental restoration materials. When discussing biocompatibility, we refer to the material’s ability to perform its desired function without eliciting any undesirable local or systemic effects in the body. The material should not cause toxic or inflammatory responses and should integrate well with the surrounding tissues.
Dentists must consider factors such as allergic reactions, sensitivity, tissue response, and the material’s overall interaction with the body. Compatibility testing, regulatory certifications, and clinical research are reliable resources to verify the biocompatibility of dental materials.
Examples of Biocompatible Dental Restoration Materials
Several dental restoration materials have proven their biocompatibility and effectiveness over the years. Here are a few examples:
Composite Resins: Dental composite resins are biocompatible materials widely used for fillings. They are aesthetically pleasing, durable, and less likely to cause allergic reactions or sensitivity.
Ceramics: Ceramic materials, including porcelain and zirconia, are biocompatible and highly aesthetic. They are used in crowns, bridges, veneers, and dental implants.
Titanium: Known for its strength and biocompatibility, titanium is the material of choice for dental implant posts.
Gold and Gold Alloys: Gold and its alloys have been used in dentistry for centuries. They are biocompatible, durable, and resistant to corrosion.
Choosing the suitable restorative material is a crucial determinant of treatment success. It’s vital to consider not only the material’s physical and aesthetic properties but also its biocompatibility. By prioritizing biocompatibility, dental professionals can enhance patient safety, improve treatment outcomes, and promote oral health.
Properties of Dental Materials and Their Impact
In dental restorations, more is needed for materials to be aesthetically pleasing – they also need to demonstrate several other properties to ensure optimal patient outcomes. From physical and mechanical attributes to their interaction with biological systems, the characteristics of dental materials play a vital role in the success of dental procedures. This section will delve into these properties, their influence on biocompatibility and clinical outcomes, and the impact of dental materials research.
Properties of Dental Materials: A Multifaceted Consideration
Dental materials must meet a stringent set of criteria to be suitable for clinical use. The physical properties include color, luster, transparency, and texture, directly contributing to the material’s aesthetic appeal. However, other crucial attributes must also be considered, including:
Mechanical Properties: Materials should exhibit strength, durability, and resistance to wear, fatigue, and fracture. These properties are paramount for the material’s longevity and the functionality of the restoration.
Thermal Properties: Dental materials should have low thermal conductivity to protect the pulp from temperature changes in the oral cavity. They should also withstand the heat generated during the setting without causing discomfort or damage to surrounding tissues.
Chemical Properties: Materials should be resistant to corrosion and degradation in the moist, acidic environment of the mouth. They should not leach harmful substances over time.
Biocompatibility and Clinical Outcomes
The properties of dental materials are intrinsically linked to their biocompatibility and clinical performance. Materials that are mechanically sound, stable in the oral environment, and cause no adverse tissue responses are more likely to be biocompatible, leading to better clinical outcomes.
Furthermore, biocompatible materials can contribute to patient comfort, a vital consideration in dentistry. Materials that have poor thermal insulation or release harmful substances can cause sensitivity, discomfort, or even pain, negatively affecting the patient’s experience.
Impact Factor and Importance of Dental Materials Research
The impact factor of dental materials research can’t be overstated. Advances in this field directly influence the quality of dental care available to patients worldwide. Continued research and development in dental materials, including biocompatible options, are crucial for improving treatment outcomes, patient satisfaction, and oral health.
Research findings published in reputable journals (identified by their high impact factor) offer dentists insights into innovative materials and techniques, contributing to improved standards of care in the field. Thus, staying updated on this research is vital for any dental practitioner aiming to provide the best possible care.
In summary, the properties of dental materials have a significant bearing on their success in dental procedures. Understanding these properties and their implications on biocompatibility and clinical outcomes is essential for dentists as they navigate the expanding array of materials available for dental restorations.
Conclusion
The world of dentistry has evolved remarkably over the years, with a significant focus on the materials used in restorative procedures. As explored in this blog, biocompatible materials play a crucial role in modern dentistry, driving both the success of dental restorations and patient satisfaction.
The Role of Biocompatibility
Biocompatibility is more than a desirable feature—it is a standard for any material used in the human body, including dental restorations. From fillings to implants, the materials must be compatible with our body’s biological systems to prevent adverse reactions, ensuring safety and optimal outcomes.
The Uses and Applications of Biocompatible Dental Materials
Biocompatible materials have demonstrated their value and efficacy throughout the various sectors of restorative dentistry, including dental fillings, impressions, composites, and implants. Their characteristics, ranging from mechanical strength to aesthetic appeal, make them ideal for numerous applications. Their continued development and evolution will undoubtedly influence the future of dentistry, offering even more possibilities for restorative procedures.
The Patient-Centric Approach in Dentistry
In the final analysis, adopting biocompatible materials emphasizes the patient-centric approach in dentistry. The choice of these materials reflects the commitment to patient safety, comfort, and satisfaction, which is, after all, the ultimate goal of any healthcare practice.
The success of dental restorations depends significantly on the materials used, and choosing biocompatible ones is the key to achieving long-term success. Understanding the significance of these materials, their properties, and how they interact with our bodies is integral for any dentist seeking to deliver the highest standard of care.
Dentistry is a field that is as much about science as it is about art. It’s about restoring not just the function but also the form, contributing to patients’ overall well-being. And in this endeavor, biocompatible materials are not just a choice—they are the standard.
SYNOPSIS:
“Discover the future of restorative dentistry in our latest blog, where we delve deep into the significance and applications of biocompatible materials. From dental fillings to implants, understand the crucial role these materials play in patient safety and satisfaction. If you’re committed to delivering exceptional care, this guide provides key insights into optimizing your dental restorations.





Leave a comment